You may have heard the term ‘instability’ in regard to musculoskeletal injuries. But what does this mean, and can we fix it?
Instability and the shoulder joint
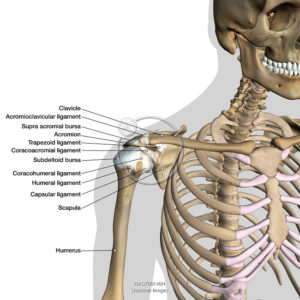
The shoulder is structured as a ball and socket joint, where the humeral head sits in the glenoid fossa. It’s kept in place by several ligaments and muscles which provide stability and mobility to the joint.
These ligaments blend to form the joint capsule which surrounds the humeral head and keeps it in place.
Instability occurs when the structures surrounding the joint (ligaments and muscles) are inadequate to maintain the humeral head in the glenoid fossa. This ‘loose’ shoulder can lead to subluxation and dislocations of the shoulder and can be associated with chronic shoulder pain or ‘dead arm’ sensation.
Ligaments of the shoulder
Types of instability
Anterior
- Instability in the front of the shoulder, the humeral head translates forwards excessively
- Often from acute dislocation or subluxation from trauma
- Common in baseball pitchers, tennis players and swimmers
Posterior
- Instability at the back of the shoulder where the humeral head translates backwards
- Can be traumatic or chronic
- Often happens from a fall on an outstretched arm
- Usually experience pain with exercises such as bench press
Multi-directional
- Generalised instability in any direction
- Usually chronic and often associated with overall ligamentous laxity e.g. hypermobile people
Dislocation vs subluxation
| Dislocation | Subluxation |
| Humeral head ‘pops out’ of glenohumeral joint and stays displaced. Requires medical assistance to relocate | Increased movement within the joint capsule or the humeral ‘pops’ out and back in automatically |
| Often associated with a fracture or labral tear | Unlikely to be associated with a fracture |
| High force or velocity injury e.g. rugby tackle | Less force required |
| High recurrence rate | High recurrence rate |
Physio management and prevention
Your physiotherapist can use a range of techniques to help reduce pain and re-gain range of motion. These often include:
- Soft tissue therapy
- Taping and bracing
- Dry needling
- Joint mobilisations – often thoracic spine
- Avoiding stretching – focus on strength immediately after and ongoing as prevention
- Ice/heat
- Modified activities of daily living
Long term management and prevention however comes from an individualised strengthening and rehabilitation program. It’s important to focus on scapula strength, rotator cuff strength and stability exercises through your shoulder range to ensure the shoulder is strong and stable in every position. These exercises vary greatly depending on your sports requirements.
Surgical intervention
If conservative management and rehabilitation fail and there are recurrent dislocations or subluxations then surgical fixation may be required. Often surgery will be required if there is an associated labral tear or lesion.

